Intro
This blog is a collection of posts related to prostate cancer, beginning with checkups, the diagnosis, subsequent surgery, and the ongoing recovery. Although your urologist will give you some reading materials to help guide you through the experience, there were many things I wish I’d known about the surgery and recovery beforehand.
Hopefully I can help you navigate the twists and turns involved in this journey so that you can be prepared for every stage of your treatment.
Monitoring
Starting in my early fifties my family doctor included a check for PSA in my blood work that accompanied regular checkups. A PSA test is a blood test used to screen for prostate cancer. The test measures the amount of prostate-specific antigen (PSA) in your blood.
When my PSA levels began to climb, I was referred to a urologist who took over and scheduled regular prostate exams.
This continued for roughly ten years as my PSA levels continued to climb. Roughly every second year a biopsy was done. This involves taking a dozen or so samples using a spring like device that impacts the prostate gland and removes a tiny amount of tissue which is analyzed. The problem with this is that none of the samples collected may be from an area of concern that could be cancerous. Also, not all parts of the prostate can be targeted for sample collection, for example the prostate gland has one side that is inaccessible because it rests against the bowel wall. One of these biopsies had a very small area that concerned my specialist and he began to keep a close eye on it.
In January 2022 my urologist informed me that my PSA readings were high enough to be concerning and suggested another biopsy, or as an alternative, a CT scan which would be scheduled at a hospital. I chose the CT scan and continue to be happy I did. It results in a complete image of the gland and in my case, a visible area showing a cancerous growth. I would recommend requesting a CT scan if you've already had a few biopsies.
Diagnosis
I can’t say I was surprised when the diagnosis came back that I definitely had prostate cancer. It seemed that this was the direction things were headed over the decade or so of monitoring, biopsies, and the eventual scan.
Still, it’s a gut punch to hear it.
If you’re going to get cancer though, prostate cancer would be the kind to have since its one of the slowest growing types. As long as detection is early, the prognosis is generally very good.
In my case there are three treatment options:
-
Radiation
The problem with this is that if your prostate cancer returns later on you can’t then do option 2. You would have to do chemotherapy. While not as invasive as surgery, there are still side effects.
-
Radical Prostatectomy and Bilateral Pelvic Lymphadenectomy
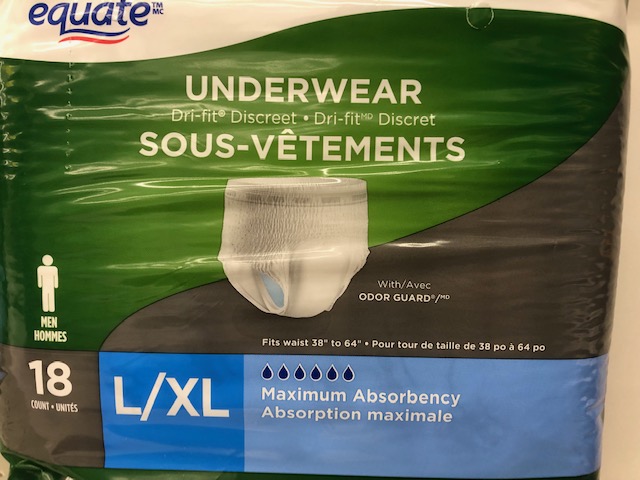
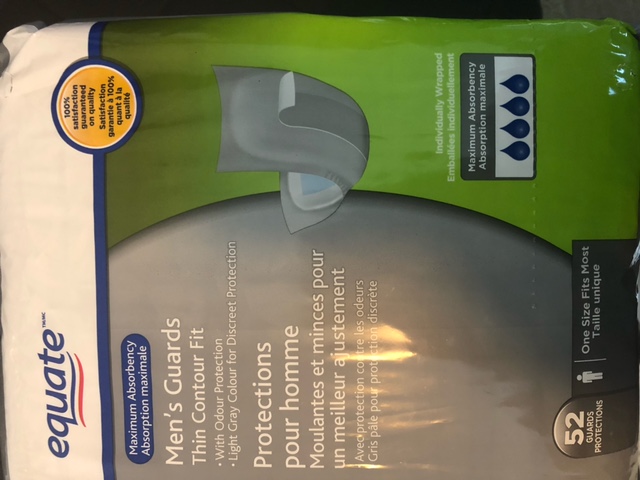
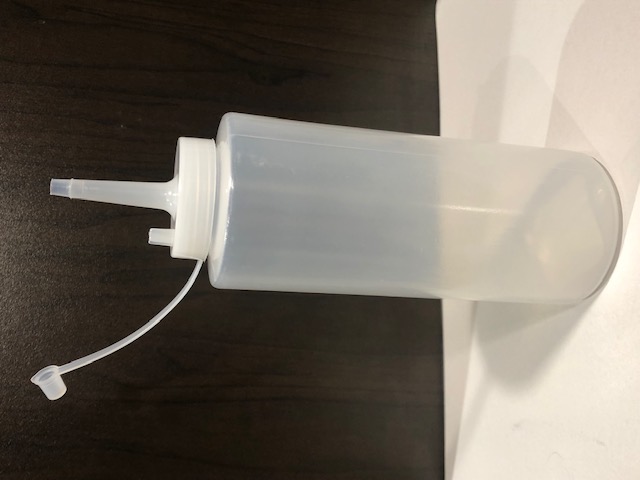
This involves the complete removal of the prostate gland as well as lymph nodes close to the prostate gland. I chose this option as it was recommended by my urologist and I liked the idea of having the cancerous growth gone! My urologist warned me though that the recovery is at least three months (no full golf swings or strenuous activity) and the first 2-3 weeks are especially tough having a catheter for two weeks is standard procedure. Expect to stay in the hospital for 4-5 days before being discharged. This is a major operation, I was in the operating room for roughly 3.5 hours and afterwards you’ll have internal stitches, external staples as well as a drain for fluid that collects around the incision.
-
Robotic-assisted Radical Proctectomy
This sounded good but was not available in Manitoba as of June 2022.
My follow up appointment where these options were presented to me was in early April. I was told that a surgery date would probably be in August or September. I remember thinking that it could be longer than that if another wave of Covid came and surgeries started getting cancelled again!
In the first week of June, I got a package in the mail indicating my surgery was scheduled for June 29. I felt relieved that I had a date soon enough that Covid might not have time to build up again, but it made for a very short golf season as our spring was so cold and wet with flooding that most courses didn’t open until the second week in May.
Still sooner was definitely better than later!